

Results: Acuity of participants at 20/20 (M=0.06 LogMAR, SD =0.1), simulated 20/80 (M=0.63, SD =0.18) and simulated 20/200 (M=0.88, SD =0.19) showed that the participants experienced simulated acuity loss with the goggles. For comparison, we included MoCA data from a sample of older adults with normal vision (n=19, Mage =74, Acuity M=0.04 logMAR, SD=0.16) or visual impairment (n=19, Mage =79, Acuity M=0.35 logMAR, SD=0.3). Only participants that scored >26 (i.e., normal cognitive function) at 20/20 were included in the analysis. The MoCA was administered following the clinical protocols. Methods: Participants (n=19) completed one of the three version of the MoCA under three conditions (20/20, simulated 20/80, simulated 20/200). Therefore we simulated visual impairments, i.e., reduced visual acuity and contrast sensitivity, in young healthy adults to determine how this impacts their scores on a measure of cognitive ability, i.e., the MoCA. But it is not clear if lowers scores on cognitive assessments are due to the assessments relying on visual stimuli, or if individuals with visual impairments are actually more likely to have cognitive impairments. Scores on cognitive assessments are typically lower for individuals with visual impairments compared to individuals with normal/corrected to normal vision.
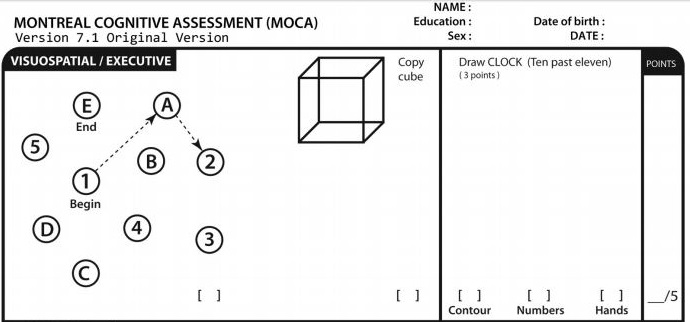
To learn more about virtual cognitive screening, please see. The College of Family Physicians of Canada and other organizations provide helpful information on setting up and optimizing telehealth approaches. To those living rurally or at a distance, balancing face-to-face with virtual visits should be considered. It is difficult to assess visuospatial abilities and to administer tests relevant to fitness to drive, such as the Trail Making A and B tests, 13 in a virtual environment.įace-to-face and virtual assessments should complement each other, with initial assessments done in office (or part virtual and part in person) and some follow-up done virtually when appropriate and feasible. The lack of visual cues during telephone assessments might also be problematic. For cognitive assessments, some patients might write down the words they have been asked to recall, thereby invalidating that aspect of memory testing. Not all families can support audiovisual assessment telephone assessment remains far more common. Telephone audio quality might be poor and patients being assessed might have hearing impairments. There are barriers to remote assessment, as family physicians have experienced during the pandemic. This means that the patient will need to access the test by printing it at home or receiving a copy in the mail.
#Blind moca pdf how to#
The authors of the MoCA have developed instructions on how to administer it virtually.
#Blind moca pdf full#
When video equipment is available and of good quality, it is possible to complete full versions of tests like the MoCA and the MMSE 12 while observing patient responses. If caregivers can be present, virtual assessment can assess for further functional loss and development of concerning symptoms. Once dementia is diagnosed, monitoring for functional loss and development of challenging behaviour or safety issues is crucial. Family members often try to help loved ones during office assessments, and monitoring this remotely might be difficult.Īs with conventional testing, physicians need to interpret the findings in the context of the patient’s vision, hearing, education level, and daily function (activities of daily living and instrumental activities of daily living).

The patient should participate without assistance, unless requested by the assessor. The environment for virtual care should be quiet and private.


 0 kommentar(er)
0 kommentar(er)
